Understanding MERS: Why Global Viral Threats Matter, Even In Michigan
In an increasingly interconnected world, understanding global health challenges is paramount, even for communities seemingly far removed from their epicenters. One such challenge is Middle East Respiratory Syndrome (MERS), a viral illness that, while originating thousands of miles away, underscores the importance of global health vigilance for every region, including the vibrant state of Michigan. While the term "Mers of Michigan" might initially bring to mind a localized issue, it serves as a crucial reminder that public health is a collective responsibility, transcending geographical boundaries.
This article delves into the complexities of MERS, exploring its origins, transmission, symptoms, and the broader implications it holds for public health worldwide. We'll utilize established scientific data to provide a comprehensive overview, emphasizing why awareness and preparedness for diseases like MERS are vital for all, from healthcare professionals to the general public, regardless of their location.
Table of Contents
- What is MERS-CoV? Unpacking the Virus
- Origins and Zoonotic Transmission: The Camel Connection
- Symptoms and Clinical Presentation: Recognizing the Signs of MERS
- Human-to-Human Transmission and Containment Efforts
- Global Surveillance and Case Data: Tracking the Spread of MERS
- Why Global Health Concerns Matter in Michigan
- Prevention and Control Strategies: Safeguarding Health
- The Future of MERS: Research and Preparedness
What is MERS-CoV? Unpacking the Virus
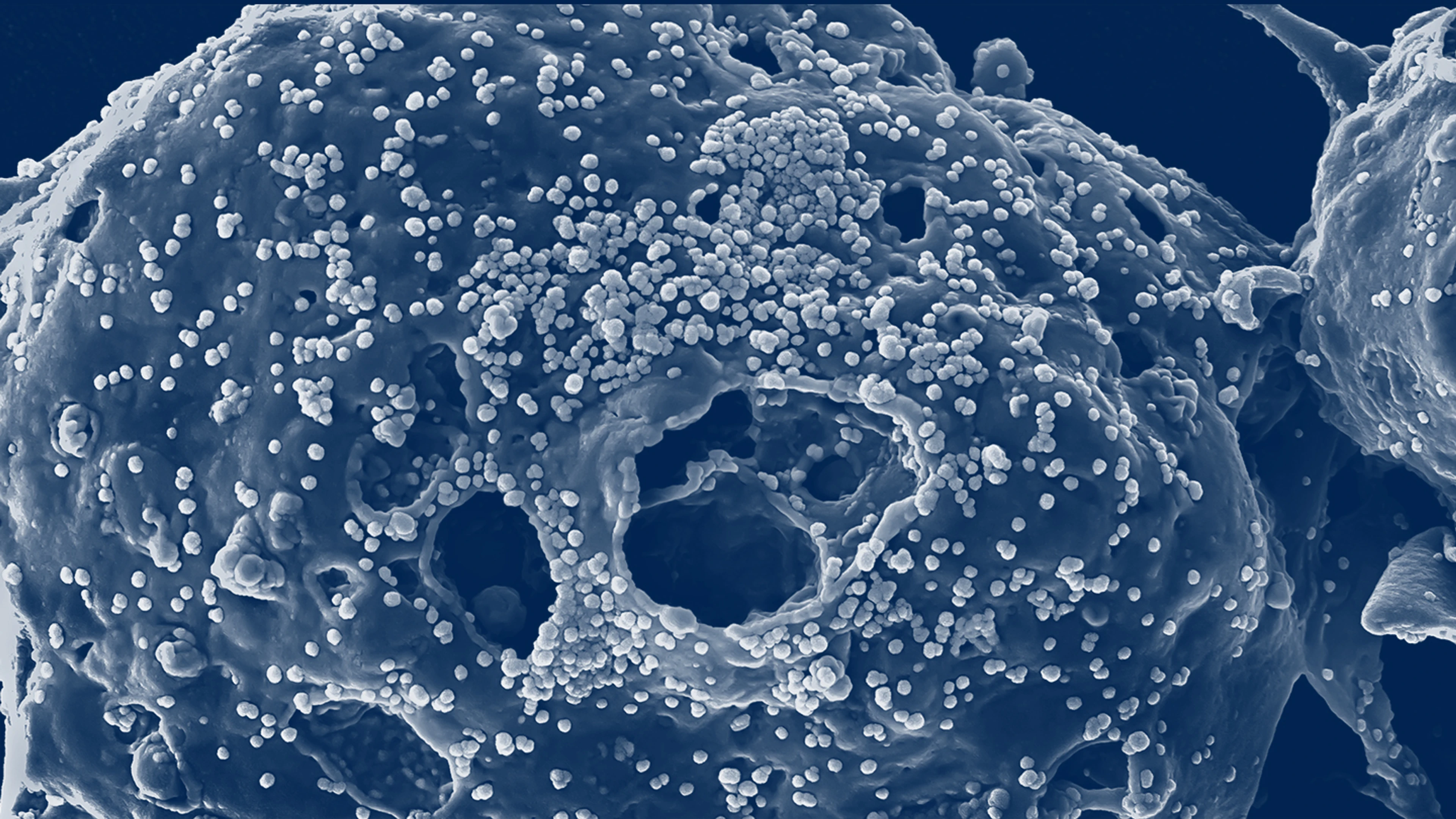
Middle East Respiratory Syndrome (MERS) is a severe viral respiratory disease caused by the Middle East Respiratory Syndrome Coronavirus (MERS-CoV). This virus, a member of the large family of coronaviruses, was first identified in Saudi Arabia in 2012. Coronaviruses are known to cause a range of illnesses, from the common cold to more severe diseases like Severe Acute Respiratory Syndrome (SARS) and Coronavirus Disease 2019 (COVID-19). MERS-CoV specifically targets the respiratory system, leading to potentially life-threatening conditions.
The identification of MERS-CoV marked a significant moment in global public health, prompting intensive research and surveillance efforts worldwide. Its emergence highlighted the constant threat posed by novel zoonotic pathogens and the critical need for rapid identification and response mechanisms. Understanding the fundamental nature of MERS-CoV is the first step in appreciating its potential impact, even on distant communities like those in Michigan.
Origins and Zoonotic Transmission: The Camel Connection
A defining characteristic of MERS is its zoonotic nature, meaning it is transmitted between animals and people. The primary animal reservoir for MERS-CoV has been identified as dromedary camels. Scientific investigations have repeatedly linked human infections to direct or indirect contact with these animals. The virus has been identified and linked to human infections in dromedaries across several countries in the Middle East and Africa, confirming their central role in the virus's ecology.
The exact mechanism of transmission from camels to humans is still being studied, but it is believed to involve close contact with infected camels or their products, such as raw camel milk or undercooked camel meat. This zoonotic jump from animals to humans is a critical aspect of MERS, differentiating it from purely human-to-human transmitted diseases and presenting unique challenges for control and prevention. The global trade and movement of animals, even those not typically found in places like Michigan, underscore the interconnectedness of animal and human health.
Symptoms and Clinical Presentation: Recognizing the Signs of MERS
The clinical presentation of MERS can vary widely, ranging from mild or asymptomatic cases to severe acute respiratory illness, often requiring intensive care. The most common symptoms include a febrile acute respiratory illness, characterized by fever, cough, and shortness of breath. Pneumonia is a common complication among those infected with MERS-CoV, often severe enough to be visible through radiological or histopathological evidence.
However, it's crucial to note that some people infected with the MERS virus have been reported to be asymptomatic, meaning they show no symptoms despite carrying the virus. This asymptomatic carriage poses a challenge for surveillance and control efforts, as infected individuals may unknowingly transmit the virus. Gastrointestinal symptoms, including diarrhea, have also been reported in some MERS patients, adding to the complexity of diagnosis. The variability in symptoms means that healthcare providers, wherever they are, must maintain a high index of suspicion, especially for individuals with relevant travel or exposure history.
Human-to-Human Transmission and Containment Efforts
While MERS is primarily zoonotic, the virus has demonstrated a limited ability to transmit between people. This human-to-human transmission typically occurs in close contact settings, such as within households or healthcare facilities. Healthcare-associated outbreaks have been a particular concern, emphasizing the need for stringent infection control measures in hospitals and clinics. The limited transmissibility between people has, to some extent, prevented the widespread global pandemics seen with other respiratory viruses.
Containment efforts for MERS have focused on early identification of cases, isolation of infected individuals, contact tracing, and rigorous infection prevention and control practices, especially in healthcare settings. These measures are crucial to break chains of transmission and prevent larger outbreaks. Global health organizations, including the World Health Organization (WHO), have played a pivotal role in coordinating these efforts, providing guidance, and supporting affected countries. The lessons learned from containing MERS outbreaks are invaluable for responding to future emerging infectious diseases, reinforcing the idea that effective public health strategies are universally applicable.
Global Surveillance and Case Data: Tracking the Spread of MERS
Since its identification, global surveillance for MERS has been a continuous effort. The WHO and collaborating institutions, including colleagues from the University of Oxford, Imperial College London, and Institut Pasteur, have meticulously tracked cases and conducted epidemiological studies. These efforts provide crucial data on the virus's prevalence, geographical distribution, and epidemiological characteristics.
For instance, these collaborative efforts have estimated that, since 2016, there have been 1,465 cases of Middle East Respiratory Syndrome. Such data is vital for understanding the trajectory of the disease, assessing risk, and informing public health policies. The ongoing surveillance highlights that while MERS may not be a daily headline in Western countries, it remains an active public health concern in regions where it is endemic. This global data serves as a constant reminder that no region, not even Michigan, is entirely isolated from the potential ripple effects of infectious diseases originating elsewhere.
Why Global Health Concerns Matter in Michigan
The concept of "Mers of Michigan" might seem counterintuitive given the virus's origins, but it encapsulates a vital truth: in today's globalized world, a health threat anywhere can become a health threat everywhere. While there haven't been significant outbreaks of MERS directly linked to Michigan, the state is not immune to the indirect impacts or the potential for imported cases. Understanding this interconnectedness is crucial for maintaining public health resilience.
The Interconnectedness of Global Travel
Michigan, like any other state, is a hub for international travel and commerce. People travel to and from the Middle East for business, tourism, and family visits. This constant movement of people means that a person infected with MERS-CoV in an endemic region could potentially arrive in Michigan before symptoms manifest or before they are diagnosed. While the limited human-to-human transmission reduces the risk of widespread community spread, the possibility of imported cases necessitates vigilance from healthcare systems and public health authorities.
Furthermore, the global supply chain, which brings goods and sometimes even animals from various parts of the world, creates additional pathways for potential exposure, even if indirect. This intricate web of connections means that a disease like MERS, seemingly confined to a specific region, demands global awareness and preparedness.
Public Health Preparedness in Michigan
For states like Michigan, preparedness for global health threats involves several layers of defense. This includes:
- Surveillance Systems: Robust systems to monitor for unusual respiratory illnesses, especially among travelers or those with relevant exposure history.
- Healthcare Capacity: Ensuring hospitals and healthcare facilities are equipped with appropriate infection control protocols, personal protective equipment (PPE), and isolation capabilities to manage potential MERS cases safely.
- Laboratory Capabilities: The ability to quickly and accurately diagnose MERS-CoV and other emerging pathogens.
- Emergency Response Plans: Pre-existing plans for rapid response, contact tracing, and public communication in the event of an imported case or limited cluster.
Education and Awareness for Michigan Residents
Empowering Michigan residents with accurate information about global health threats like MERS is a critical component of public health. This includes:
- Educating travelers about health risks in their destinations and precautions to take.
- Informing healthcare providers about symptoms and travel history to consider MERS in their differential diagnosis.
- Promoting general hygiene practices, such as handwashing and respiratory etiquette, which are effective against many respiratory viruses.
Prevention and Control Strategies: Safeguarding Health
Effective prevention and control strategies are paramount in mitigating the risk of MERS. For individuals, particularly those traveling to or residing in affected regions, avoiding direct or indirect contact with dromedary camels is a key recommendation. This includes refraining from consuming raw camel milk or undercooked camel meat. Practicing good hand hygiene, such as frequent handwashing with soap and water, is also crucial, especially after contact with animals or in healthcare settings.
For healthcare professionals, strict adherence to infection prevention and control measures is non-negotiable. This involves using standard precautions for all patients, and contact and droplet precautions for suspected or confirmed MERS cases. These measures are designed to protect both healthcare workers and other patients from potential transmission. Public health authorities, both globally and locally, continue to emphasize these strategies as the frontline defense against MERS-CoV.
The Future of MERS: Research and Preparedness
Research into MERS-CoV continues globally, focusing on understanding its epidemiology, developing effective treatments, and creating vaccines. While the virus has demonstrated limited ability to transmit between people compared to other coronaviruses, the potential for mutation and increased transmissibility always exists. Therefore, ongoing scientific inquiry and surveillance are vital to stay ahead of the curve.
The global health community, including institutions that provided data for our understanding of MERS, remains committed to monitoring the virus and supporting affected countries. For regions like Michigan, this means staying connected to global health intelligence, adapting local preparedness plans based on new scientific findings, and continuing to invest in public health infrastructure. The lessons from MERS, and indeed from other pandemics, reinforce the idea that a proactive, globally aware approach to public health is the strongest defense against future viral threats. The "Mers of Michigan" narrative, therefore, evolves from a potential local concern to a powerful metaphor for universal vigilance and preparedness.
In conclusion, while Middle East Respiratory Syndrome is primarily associated with specific regions and animal hosts, its existence serves as a potent reminder of our interconnected world. The concept of "Mers of Michigan" isn't about an endemic local outbreak, but rather about the essential need for every state and every community to be aware, prepared, and resilient in the face of global health challenges. By understanding the science behind MERS, supporting public health initiatives, and fostering a culture of preparedness, we can collectively safeguard our well-being.
Do you have thoughts on how global health issues impact your local community? Share your insights in the comments below, or explore our other articles on public health and infectious disease preparedness to learn more.

MERS | Causes, Symptoms & Treatment | Britannica
MERS | CEPI

Mers Tran - Knowles Teacher Initiative